Fasting. Authentication. Inquire. Repeat

Cliff
One of many elephants in the room of health and fitness. Is insulin resistance (IR) supposed to be protective?(Update August 2nd 2023: more citations added!)
Welcome to what is perhaps the least (but not the first) visited independent dialogues on alternative nutritional science, in the lens of inaccessibility.
Here, we are discussing one of many elephants (or dogmas) in the room ~ everything about Insulin Resistance (IR) = "bad". This stems from the current consensus, which firmly believe that Free Fatty Acid (FFAs) release, has been the central mechanism behind IR (Sears B & Perry M 2015) & (Bergman RN & Ader M 2000) and its associated signs~ impaired glucose uptake to lean tissue, upregulate cortisol synthesis. Before then consequently ~ every disease outcomes one can think of ~ obesity, endocrine / thyroid dysregulation, IBD, IBS, T2D / type 2 diabetes, CVD / cardiovascular disease, alzheimer's, stroke, PCOS, to name a few.
Cliff Notes
- Insulin Resistance (IR) can be interpreted as either Pathological or Physiological. The latter ~ Physiological ~ is arguably constructive, given the right context in terms of age (particularly puberty), and stage of life (especially pregnancy status in women). Physiological here is also at times referred to as "Adaptive Glucose Sparing" or "Fasting induced Insulin Resistance" (Tzintzas A et al. 2007).
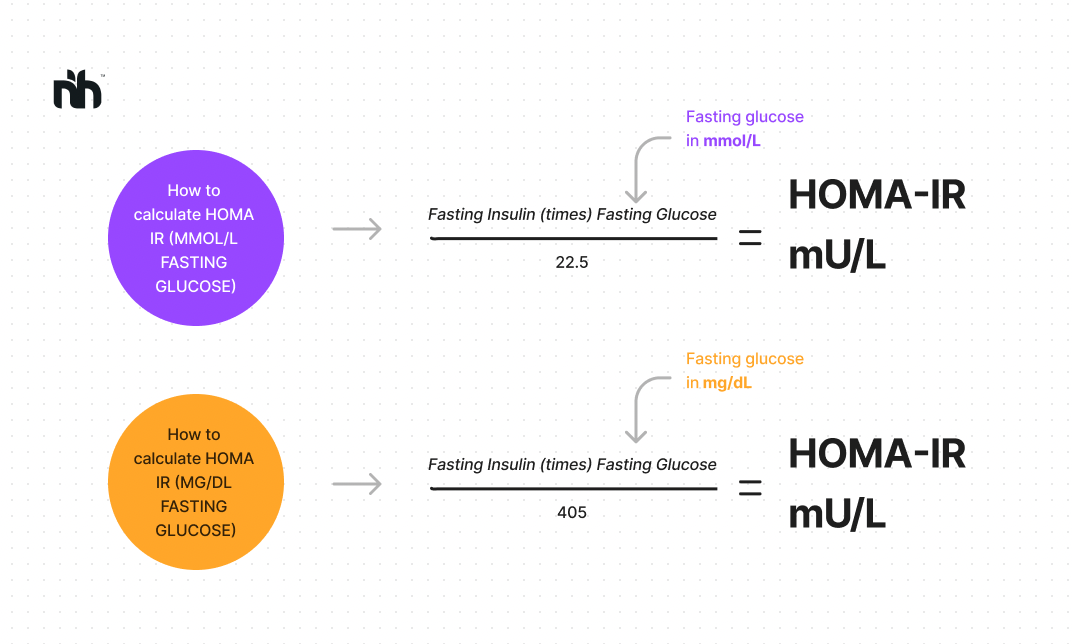
- Besides from lifestyle modifications, exercise / fitness, environmental and psychosocial / structural access to wholefoods, nutrients support, and education - etiology(s) and mechanistic causation behind IR remains widely contested, broad and nuanced. However an objective marker to this remains in agreement in almost all circles ~ to be that of an excess insulin presence in the blood ~ aka. hyperinsulinemia. This is diagnose-able by HOMA-IR test, or known as as Homeostatic Model Assessment of Insulin Resistance. It measures how much endogenous Insulin is required to bring the ideal reference ranges and is increasingly thought to be more important than fasted glucose reading tests alone (Cooper JD et al. 2022), (Keskin M et al. 2005), . & (Ramesh R et al. 2022) Below is a reminder (my illustration/graphic) at calculating HOMA-IR.
Generally, higher HOMA-IR ~ suggests hyperinsulinemia as more presence of insulin is required for euglycemia / homeostasis, hence, more potential stress on the pancreas to release more insulin and thereby exhausting its Beta cells in doing so. Lower = considered ideal, as it suggests only small amount of insulin required for glucose homeostasis; arguably less demand on the pancreas.
....And now - the cliff quotes from the key studies.
Please note that all bolding(s) and/or underlining are my own deliberate emphasis.
- "Reversing impaired insulin sensitivity has been suggested as treatment for heart failure. However, recent clinical evidence suggests the opposite." (Taegtmeyer H et al. 2013)
- We propose that in the heart, insulin-sensitizing agents result in a breakdown of the defenses leading to cytotoxic damage. In contrast, a normalization of fuel supply should either prevent or reverse the process. This is a new perspective to a vexing physiological and clinical problem." (Taegtmeyer H et al. 2013)
- “Our findings highlight the ability of the β-cell to promptly fine-tune insulin production and secretion to transition from a protective state during fasting to one that meets the acute physiological metabolic demand presented by refeeding.” Boland BB et al. 2018.
- “[...] we propose that IR, particularly in this high-risk subgroup, is a defense mechanism that protects critical tissues of the cardiovascular system from nutrient-induced injury. Overriding IR in an effort to lower plasma glucose levels, particularly with intensive insulin therapy, could therefore be harmful.” Nolan CJ et al. 2015
- “Insulin resistance may be an appropriate response to nutrient excess, but the cellular sensors that link these parameters remain poorly defined." (Hoehn KL et al. 2009)
- "Using mice with skeletal musclespecific ablation of the insulin receptor gene (MIRKO), we addressed this paradox by demonstrating that insulin signaling in skeletal muscles specifically mediated cross talk with the heart, but not other metabolic tissues, to prevent cardiac dysfunction in response to metabolic stress. Despite severe hyperinsulinemia and aggregating obesity, MIRKO mice were protected from myocardial insulin resistance, mitochondrial dysfunction, and metabolic reprogramming in response to diet-induced obesity." (Jia D. et al. 2021)
Overriding existing homeostasis : possible danger.
“Overriding” here refers to clinically bypassing or surpassing the body’s own / existing insulin regulation. Usually by insulin administration and/or injection. Studies are gaining traction that it is caloric excess, that prompts cellular response to therefore resist any partitioning or storing any energy, into fat cells. Hence, a new emerging thought that implies IR as a protective response.
- “Insulin thus ensures efficient storage of energy so that it is available for mobilization during fasting, when insulin levels are low. However, chronic overnutrition, undernutrition, or other states of cellular stress can generate insulin resistance (Biddinger and Kahn, 2006, Doria et al., 2008, Olefsky and Glass, 2010, Saltiel, 2001), which is advantageous when energy mobilization is needed.”
Saltiel AR 2012 - “As a consequence of this premise, they argue against intensive insulin treatment as an approach to override IR with the final goal of satisfactory blood glucose control in obese subjects unlikely to correct positive energy balance through lifestyle interventions (1).”
(A comment on Nolan Et al. 2015)
Insulin Sensitive = more fat gain? + more "myocardial" lipids?
If we are talking about IR’s effect with straight-face value - Insulin Resistance seem to be correlated with less weight gain upon glucose disposal test.
- “Insulin-resistant subjects gained less weight than insulin-sensitive subjects (3.1 vs. 7.6 kg, P less than 0.0001).” (Swinburn AB et al. 1991)
- “Insulin resistance, whether or not it was corrected for the initial body weight, was associated with a lower rate of weight gain than insulin sensitivity. This relationship was independent of age, sex, and 24-h energy expenditure.” (Swinburn AB et al. 1991)
Insulin administration may be damaging to the heart. How does "80% increase - of myocardial lipids" as an outcome, sound? That I certainly don’t find comfortable.
- “We propose that IR protects critical tissues, such as the heart, from nutrient-induced damage in this subgroup and that “approaches” to intensively lower blood glucose that override IR (e.g., high-dose insulin therapy) will cause them harm.“ Nolan et al. 2015
- “(…) treatment of patients with T2D with 10 days of exogenous insulin increased the myocardial lipid content by 80%, the level of which was positively associated with the initial mean glucose concentration (18)." Nolan et al. 2015
- “Although decreasing insulin resistance is a major strategy to relieve some demands on pancreatic beta cells to increase insulin secretion in type 2 diabetes mellitus, it may be associated with less protection of other organs.”Barzilai N et al. 2012
...And what about Longevity?
Surprisingly - insulin resistance may yet play a role in longevity, involving chiefly among such series of processes - MTOR inhibition.
- “Signaling downregulation of the target for rapamycin and more recently of its mammalian equivalent extends life spans in multiple species, by multiple mechanisms such as enhanced autophagy and decreased mitochondrial production of reactive oxygen species. Interestingly, reduction of mTOR signaling is associated with decreased insulin sensitivity (12).”Barzilai N et al. 2012
Love it or hate it - animal studies have their own advantages. Here in this mice study it appears that an increase in longevity is correlated only in insulin insensitive male mice. Again as reminder - bolded lines are my own emphasis:
- "Given the pathological sequelae of diabetes, it seems counterintuitive that reducing insulin sensitivity on mammals would increase life span. However, some models of impaired insulin signaling are associated with increased longevity or resistance to life-threatening oxidative stress." (Nelson JF et al. 2012).
- "We therefore measured the life span of mice lacking either insulin receptor substrate (IRS) 1 or 2, the major intracellular effectors of the IIS receptors. Our provisional results indicate that female Irs1-/- mice are long-lived. Furthermore, they displayed resistance to a range of age-sensitive markers of aging including skin, bone, immune, and motor dysfunction. These improvements in health were seen despite mild, lifelong insulin resistance. " (Selman, C. 2008)
- "It has been well established that insulin resistance is associated with metabolic syndrome or diabetes resulting in higher mortality.1–6 However, recently increasing evidence has shown that blocking insulin action results in greater longevity in various life forms such as yeast, Caenorhabditis elegans, Drosophila, and vertebrate including primates.1,2,7 Therefore, it appears that the insulin paradox exists." ~ (Koshiyama H. 2012)
For those unaware, "Longevity" as a general buzzword is something I sometimes thread with caution. Sometimes I do believe and align in their importance. Yet other times, questionable that I still leave room for my own doubts. Sex / libido / reproductive health for instance, has been a compromised outcome of longevity, as discussed in a podcast guest interview (Simon Hill / The Proof).
What do others think?
Almost all low carbohydrate advocates; Dr Ted Naiman, Dr. Paul Saladino, Peter Dobromylskyj, Dr. Benjamin Bikman all share a common defense that insulin resistance, at least from the Physiological context ~ is a deserved function.
For many years I am also open to many other skeptical views. Chiefly among them Dr. Raymond Peat ,who recently and sadly passed away, despite polar opposing views against low carbohydrate and intermittent fasting in general, interestingly wrote / came with the following responses:
- “Some of the worst effects of “diabetes,” including retinal damage, are caused or exacerbated by insulin itself.”
- “The very rapid rise of blood sugar stimulates massive release of insulin, and rapidly converts much of the carbohydrate into fat.”
- In a guest podcast feature with Strong Sista's (14:04) ~ when asked for clarity whether insulin resistance in the fat cells is the hypothetically ideal state (in tangent to the topic of PUFAs and Metabolism) ~ Dr. Peat's response was "yes".
For courtesy, I do not aim to share "as many names" here. Citations and references above alone should confer sufficient further reading should anyone has the time to do more introspection at their own ends.
Conclusion.
As we can see, this is still complicated.
If we can just able to "self-direct" our own biochemistry, that is "telling" our own cells to become resistant only on certain cells, but not others (In this case lean muscle cells insulin sensitivity, but not fat cells) that would be ideal. Alas, life is not that simple.
This counter argument is not a 1:1 “attack” or “critique” against widely accepted view that insulin resistance is confirmed, as "bad". I admit there are numerous other "functions", besides IR, that may very well impact mortality more or if not worse than IR alone. Or perhaps combinations, with many other unknown(s). I do not know.
But I believe that metabolism adjusts overtime, and that it is up to us to work with, not against these dynamics. I believe we are obligated to respond as a function to likewise contend with our life's dynamics, stressors and circumstances. And whatever that function is, deserves empathy before we can judge, semantically.
At the end of the day, what matters is living your own life and ably respond / ably surpass against scarcity. This is what I argue for as a case through Fasting and Refeeding.
I am open to any hypothesis. So long as it is not shoved down my throat. Having both arguments evenly presented on the table is what makes Science (and life in general) that much more interesting.
AW.